Resolving trapdoor phenomenon without secondary procedure after forehead flap on medial canthal region
Accepted: 8 February 2023
HTML: 8
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
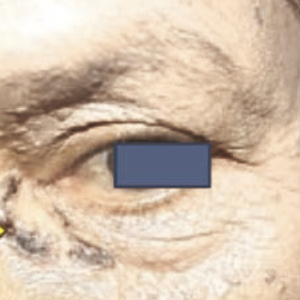
Herein, we present a case of basal cell carcinoma in a 59-yearold woman. It presented with painless itchy, black, gradually enlarged patches which were easily bled under her left eye since three years ago. A dermatological examination of the left medial canthus region obtained hyperpigmented plaques (2x0.8x0.1 cm) with uneven skin texture, irregular borders, and erosion on the center of the lesion. We performed forehead flap technique surgery followed by eight-month monitoring, resulting in a satisfying outcome in both function and appearance. The thinning technique and adjusting the flap size from the forehead area to the medial canthus should be as thin as possible to avoid differences in skin thickness and post-reconstruction hypertrophic scars. A bulging appears on the surgical site a month after the procedure, known as the trapdoor phenomenon, on the 8th month of followup, the trapdoor phenomenon disappeared.
Tang J, Epstein E, Oro A. Basal cell carcinoma and basal cell nevus syndrome. In: Goldsmith LA, Katz SI, Gilchrest BA, et al. Fitzpatrick's Dermatology in General Medicine, 9th edition: United States: The McGraw-Hills Companies. 2019;2:1884-91.
Mawardi P, Kalim H, Kalim KH, et al. Mid-face location of primary basal cell carcinoma related to cancer aggressiveness. Asian Pac J Trophy Dec 2016;6:650-3.
Martens M, Seebode C, Lehmann J, Emmert S. Photocarcinogenesis and skin cancer prevention strategies: An Update. Anticancer Res 2018;38:1153-8.
Rubik AI, Chen EH, Ratner D. Basal-call carcinoma. N Eng J Med 2005;353:2262-9.
Bimo AT, Sulistyaningsih S, Dharmawan N, Julianto J. Histologically confirmed basal cell carcinoma profile at dermatology and venereology department of Dr. Moewardi hospital in October 2008 – May 2013. Jurnal Medika Moewardi 2013;4:33-6.
Ogino A, Onishi K, Okada E, Nakamichi M. Medial canthal reconstruction with multiple local flaps. J Plas Reconstr Aesthet Surg J 2017;15:4-9.
Chao Y, Xin X, Jiangping C. Medial canthal reconstruction with combined glabellar and orbicularis oculi myocutaneous flaps. J Plas Reconstr Aesthet Surg J 2010;63:1624-8.
Amici JM. Hypertrophie cicatricielle précoce post-chirurgicale de la région nasale: intérêt des injections de corticoïde retard [Early hypertrophic scar after surgery on the nasal region: value of long-acting corticosteroid injections]. Ann Dermatol Venereol 2014;141:7-13.
Feng H, Christman MP, Bloom BS, et al. Treatment of Trapdoor Deformity Using Erbium-doped Yttrium Aluminum Garnet Laser. Plast Reconstr Surg Glob Open 2019;7:e2445.
Hayat N, Jan S, Aslam S, Asghar MS. Outcomes of Propeller Flap in Eyelid Reconstruction. Cureus 2021;13:e14509.
Rahpeyma A, Khajehahmadi S. The place of nasolabial flap in orofacial reconstruction: A review. Ann Med Surg (Lond) 2016;12:79-87.
Rajak SN, Huilgol SC, Murakami M, Selva D. Propeller flaps in eyelid reconstruction. Eye (Lond) 2018;32:1259-64.
Zhang W, Xie WG, Zhang WD, et al. [Expanded flaps with vascular anastomosis for the treatment of scar contracture deformities of extensively burned patients]. Zhonghua Shao Shang Za Zhi 2019;35:410-6.
Leibovitch I, Huilgol SC, Hsuan JD, et al. Incidence of host site complications in periocular full thickness skin grafts. Br J Ophthalmol 2005;89:219-22.
Hari I, Nicholas B, Salib, Emmanuel G. The LN Flap for Nasal Defect Reconstruction: An 84-case Experience with a Novel Technique. PRS - Global Open 2021;9:e3526.
Baxter JM, Patel AN, Varma S. Facial basal cell carcinoma. Br Med J 2012;345:37-42.
Baker S. Reconstruction of the Nose. In: Baker SR, editor. Baker locals flap in Facial Reconstruction. 4th Edition. British: Mosby Elsevier. 2021:415-74.
Kim H, Na C, Shin B. A statistical study of cutaneous basal cell carcinoma and squamous cell carcinoma in Gwangju city and Chonnam province (2006-2010). Korean J Dermatol 2011.
Kim G, Bae YC, Kim JH, et al. Usefulness of the orbicularis oculi myocutaneous flap in periorbital reconstruction. Arch Craniofac Surg 2018;19:254-9.
Karian L, Datiashvili RO. Combination of glabellar and V-Y cheek advancement flaps for large skin defects of the median canthal area. J Surg Open Access 2016;2:1-3.
Trakatelli M, Morton C, Nagore E, et al. Update of the European guidelines for basal cell carcinoma management. Eur J Dermatol 2014;24:312-29.
Costin BR, Poblete C. Reconstruction of medial canthal defects. In: Levine MR, Allen RC, editor. Manual of Oculoplastic Surgery. 5th Edition. United States: Springer. 2018:363-79.
Copyright (c) 2023 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.





 https://doi.org/10.4081/dr.2023.9590
https://doi.org/10.4081/dr.2023.9590



