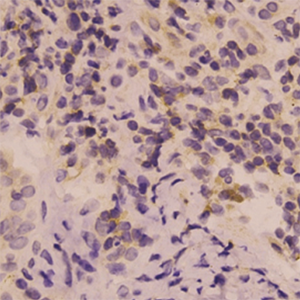
Immunohistochemical expression of interleukin β in papule biopsies from patients with acne vulgaris
HTML: 17
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Acne vulgaris is the most common inflammatory disease of the skin. IL-1β has been found in acne lesions and is a promising target for therapy, but the evidence is limited. Therefore, this study was conducted to investigate the immunohistochemical expression of IL-1β in papule biopsies of inflammatory acne and its association with disease severity. This study involved 20 patients with acne vulgaris (13 females, median age: 22 years). Samples were taken using punch biopsy. Immunohistochemical IL-1β expression was semi-quantitatively assessed as absent, mild, moderate or strong. Disease severity was evaluated according to the Global Acne Grading System (GAGS). There were 7 patients with mild disease and 11 patients with moderate disease. Median GAGS score was 20. Mild and moderate accounted for 65% and 30% for dermal IL-1β expression, 60% and 40% for epidermal expression, and 70% and 15% for perifollicular expression. Moderate-strong perifollicular expression had significant higher GAGS score than absent-mild expression (median: 22 versus 16). This study shows the elevated immunoreactivity of IL-1β in papule biopsies of inflammatory acne vulgaris. The levels of IL-1β expression also correlates with disease severity. IL-1β could be a good candidate for targeting treatment of acne vulgaris.
Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet 2012;379:361-72. DOI: https://doi.org/10.1016/S0140-6736(11)60321-8
Leeming JP, Holland KT, Cuncliffe WJ. The microbial colonization of inflamed acne vulgaris lesions. Br J Dermatol 1988;118:203-8. DOI: https://doi.org/10.1111/j.1365-2133.1988.tb01775.x
Leyden JJ, McGinley KJ, Vowels B. Propionibacterium acnes colonization in acne and nonacne. Dermatology 1998;196:55-8. DOI: https://doi.org/10.1159/000017868
Bojar RA, Holland KT. Acne and Propionibacterium acnes. Clin Dermatol 2004;22:375-9. DOI: https://doi.org/10.1016/j.clindermatol.2004.03.005
Kurokawa I, Danby FW, Ju Q, et al. New developments in our understanding of acne pathogenesis and treatment. Exp Dermatol 2009;18:821-32. DOI: https://doi.org/10.1111/j.1600-0625.2009.00890.x
Kistowska M, Gehrke S, Jankovic D, et al. IL-1β drives inflammatory responses to propionibacterium acnes in vitro and in vivo. J Invest Dermatol 2014;134:677-85. DOI: https://doi.org/10.1038/jid.2013.438
Brenner M, Ruzicka T, Plewig G, et al. Targeted treatment of pyoderma gangrenosum in PAPA (pyogenic arthritis, pyoderma gangrenosum and acne) syndrome with the recombinant human interleukin-1 receptor antagonist anakinra. Br J Dermatol 2009;161:1199-201. DOI: https://doi.org/10.1111/j.1365-2133.2009.09404.x
Braun-Falco M, Kovnerystyy O, Lohse P, Ruzicka T. Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH)--a new autoinflammatory syndrome distinct from PAPA syndrome. J Am Acad Dermatol 2012;66:409-15. DOI: https://doi.org/10.1016/j.jaad.2010.12.025
Wendling D, Prati C, Aubin F. Anakinra treatment of SAPHO syndrome: short-term results of an open study. Ann Rheum Dis 2012;71:1098-100. DOI: https://doi.org/10.1136/annrheumdis-2011-200743
Doshi A, Zaheer A, Stiller MJ. A comparison of current acne grading systems and proposal of a novel system. Int J Dermatol 1997;36:416-8. DOI: https://doi.org/10.1046/j.1365-4362.1997.00099.x
Zaenglein AL, Graber EM, Thiboutot DM. Acne Vulgaris and Acneiform Eruptions. Fitzpatrick's dermatology in general medicine. 8th ed, 2012:1391-418.
Jeremy AH, Holland DB, Roberts SG, Thomson KF, Cunliffe WJ. Inflammatory events are involved in acne lesion initiation. J Invest Dermatol 2003;121:20-7. DOI: https://doi.org/10.1046/j.1523-1747.2003.12321.x
Qin M, Pirouz A, Kim MH, et al. Propionibacterium acnes Induces IL-1β secretion via the NLRP3 inflammasome in human monocytes. J Invest Dermatol 2014;134:381-8. DOI: https://doi.org/10.1038/jid.2013.309
Girardin SE, Boneca IG, Viala J, et al. Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem 2003;278:8869-72. DOI: https://doi.org/10.1074/jbc.C200651200
Graham GM, Farrar MD, Cruse-Sawyer JE, et al. Proinflammatory cytokine production by human keratinocytes stimulated with Propionibacterium acnes and P. acnes GroEL. Br J Dermatol 2004;150:421-8. DOI: https://doi.org/10.1046/j.1365-2133.2004.05762.x
Copyright (c) 2022 the Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.





 https://doi.org/10.4081/dr.2022.9444
https://doi.org/10.4081/dr.2022.9444



