Diffuse cutaneous mastocytosis masquerading as linear IgA bullous dermatosis of childhood
Accepted: 27 January 2021
HTML: 26
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
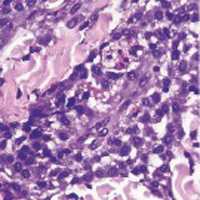
Diffuse cutaneous mastocytosis is a rare form of cutaneous mastocytosis that can appear in heterogeneous clinical presentations, including eruption of papules, erythematous plaques, blisters, and erythroderma. We report a 1.5- year-old boy who presented with itchy wheals and blisters spreading on his body. The patient was initially managed as a linear IgA bullous dermatosis of childhood because of the similarity of clinical symptoms and the presenting of linear IgA deposits at the basement membrane. Due to the development of urticarial plaque after the resolution of the blisters, the diagnosis of diffuse cutaneous mastocytosis was made based on clinical, histopathological (hematoxylin-eosin, Giemsa, and toluidine blue staining), and direct immunofluorescent examinations (IgA, IgG, IgM, C3). The symptoms were improved following antihistamines and oral corticosteroid treatment.
Ben-Amitai D, Metzker A, Cohen HA. Pediatric cutaneous mastocytosis : a review of 180 Patients. Isr Med Assoc J 2005;7:320–2.
Nettleship E. Rare form of urticaria. Br Med J 1869;2:323–4.
Brockow K. Epidemiology, prognosis, and risk factors in mastocytosis. Immunol Allergy Clin North Am 2014;34:283–95. DOI: https://doi.org/10.1016/j.iac.2014.01.003
Méni C, Bruneau J, Georgin-Lavialle S, Le Saché de Peufeilhoux L, Damaj G, Hadj-Rabia S, et al. Paediatric mastocytosis: a systematic review of 1747 cases. Br J Dermatol 2015;172:642–51. DOI: https://doi.org/10.1111/bjd.13567
Neri I, Guareschi E, Guerrini V, Patrizi A. Familial teleangiectasia macularis eruptiva perstans. Pediatr Dermatol 2005;22:488–9. DOI: https://doi.org/10.1111/j.1525-1470.2005.00123.x
Valent P, Akin C, Sperr WR, Horny H-P, Metcalfe DD. Mast cell proliferative disorders: current view on variants recognized by the World Health Organization. Hematol Oncol Clin North Am 2003;17:1227-41. DOI: https://doi.org/10.1016/S0889-8588(03)00089-3
Theoharides TC, Valent P, Akin C. Mast Cells, mastocytosis, and related disorders. N Engl J Med 2015;373:163–72. DOI: https://doi.org/10.1056/NEJMra1409760
Komi DEA, Rambasek T, Wöhrl S. Mastocytosis : from a molecular point of view. Clin Rev Alerg Immunol 2017;54:397-411. DOI: https://doi.org/10.1007/s12016-017-8619-2
Wolff K, Komar M, Petzelbauer P. Clinical and histopathological aspects of cutaneous mastocytosis. Leuk Res 2001;25:519–28. DOI: https://doi.org/10.1016/S0145-2126(01)00044-3
Alvarez-Twose I, Vañó-Galván S, Sánchez-Muñoz L, Morgado JM, Matito A, Torrelo A, et al. Increased serum baseline tryptase levels and extensive skin involvement are predictors for the severity of mast cell activation episodes in children with mastocytosis. Allergy 2012;67:813–21. DOI: https://doi.org/10.1111/j.1398-9995.2012.02812.x
Lange M, Zawadzka A, Schrörs S, Słomka J, Ługowska-Umer H, Nedoszytko B, et al. The role of serum tryptase in the diagnosis and monitoring of pediatric mastocytosis: a single-center experience. Postepy Dermatol Alergol 2017;34:306–12. DOI: https://doi.org/10.5114/ada.2017.69308
Haneef NS, Ramachandra S, Metta AK, Srujana L. Chronic bullous disease of childhood with IgG predominance: What is the locus standi? Indian J Dermatol 2012;57:285–7. DOI: https://doi.org/10.4103/0019-5154.97670
Zone JJ, Egan CA, Taylor TB, Meyer LJ. IgA autoimmune disorders: development of a passive transfer mouse model. J Investig Dermatology Symp Proc 2004;9:47–51. DOI: https://doi.org/10.1111/j.1087-0024.2004.00840.x
Slavescu KC, Chiorean R, Danescu, S, Bota M, Rogojan L, Baican A. Diffuse cutaneous bullous mastocytosis with IgM deposits at dermo–epidermal junction. J Cutan Pathol 2015;43:263–9. DOI: https://doi.org/10.1111/cup.12635
Cardet JC, Akin C, Lee MJ. Mastocytosis: update on pharmacotherapy and future directions. Expert Opin Pharmacother 2013;14:2033–45. DOI: https://doi.org/10.1517/14656566.2013.824424
Worobec AS. Treatment of systemic mast cell disorders. Hematol Oncol Clin North Am 2000;14:659–87. DOI: https://doi.org/10.1016/S0889-8588(05)70301-4
Klaiber N, Kumar S, Irani AM. Mastocytosis in children. Curr Allery Asthma Rep 2017;17:80. DOI: https://doi.org/10.1007/s11882-017-0748-4
Bulat V, Mihić LL, Situm M, Buljan M, Blajić I, Pusić J. Most common clinical presentations of cutaneous mastocytosis. Acta Clin Croat 2009;48:59–64.
Cook EB, Stahl JL, Barney NP, Graziano FM. Mechanisms of antihistamines and mast cell stabilizers in ocular allergic inflammation. Curr Drug Targets Inflamm Allergy 2002;1:167–80. DOI: https://doi.org/10.2174/1568010023344733
Belvisi MG. Regulation of inflammatory cell function by corticosteroids. Proc Am Thorac Soc 2004;1:207–14. DOI: https://doi.org/10.1513/pats.200402-002MS
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.





 https://doi.org/10.4081/dr.2021.9021
https://doi.org/10.4081/dr.2021.9021



