Atopic dermatitis: a brief review of recent advances in its management
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
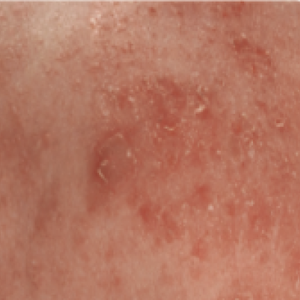
Atopic dermatitis (AD) is a common inflammatory skin disorder characterized by recurrent eczematous lesions and intense itching. The disorder affects people of all ages and ethnicities, has a substantial psychosocial impact on patients and relatives, and is the leading cause of the global burden of skin diseases. Atopic dermatitis is associated with an increased risk of multiple comorbidities, including food allergies, asthma, allergic rhinitis, and mental health disorders. The pathophysiology is complex and involves a strong genetic predisposition, epidermal dysfunction, and T-cell-driven inflammation. Although type-2 mechanisms are dominant, there is increasing evidence that the disorder involves multiple immune pathways. Until recently, the management of AD rested mainly on the judicious use of emollients, topical steroids, and topical calcineurin inhibitors in the majority of patients, and systemic immunosuppressants were advocated in severely diseased patients. However, in the last few years, new therapeutic strategies have been designed and developed to target the various steps in the chain of molecular events that lead to the AD phenotype. This review highlights the recent advancements in the management of AD.





 https://doi.org/10.4081/dr.2023.9678
https://doi.org/10.4081/dr.2023.9678